We’re living longer than ever before - and that’s a good thing. But what happens when a global rise in life expectancy outpaces our ability to care for an aging population?
Welcome to the longevity crisis.
As healthcare systems around the world stretch to support the needs of older adults, it’s clear that longevity - once a marker of progress - has become a central challenge reshaping healthcare delivery, funding, and innovation. In this article, we explore how this shift is changing healthcare, and what it means for older adults, caregivers, and the future of aging.
What Is the Longevity Crisis?
The longevity crisis refers to the mounting pressure healthcare systems face as global populations age rapidly. By 2050, it’s estimated that 1 in 6 people globally will be over the age of 65, up from 1 in 11 in 2019 (WHO).
This demographic shift - driven by lower birth rates, better living standards, and medical advances - creates a situation where:
- There are fewer working-age people to support healthcare systems
- There’s an increased prevalence of chronic diseases like dementia, heart disease, and diabetes
- Existing healthcare models, often hospital- and crisis-based, aren’t equipped to support long-term, proactive care for aging populations
How Healthcare Is Being Reshaped
1. From Reactive to Preventative Care
Traditional healthcare systems have focused on treating illness after it appears. But with more people living longer - and with multiple chronic conditions - there’s a growing shift toward preventative care and early intervention.
Examples include:
- Wearable health devices that track vitals
- Fall detection and remote monitoring systems
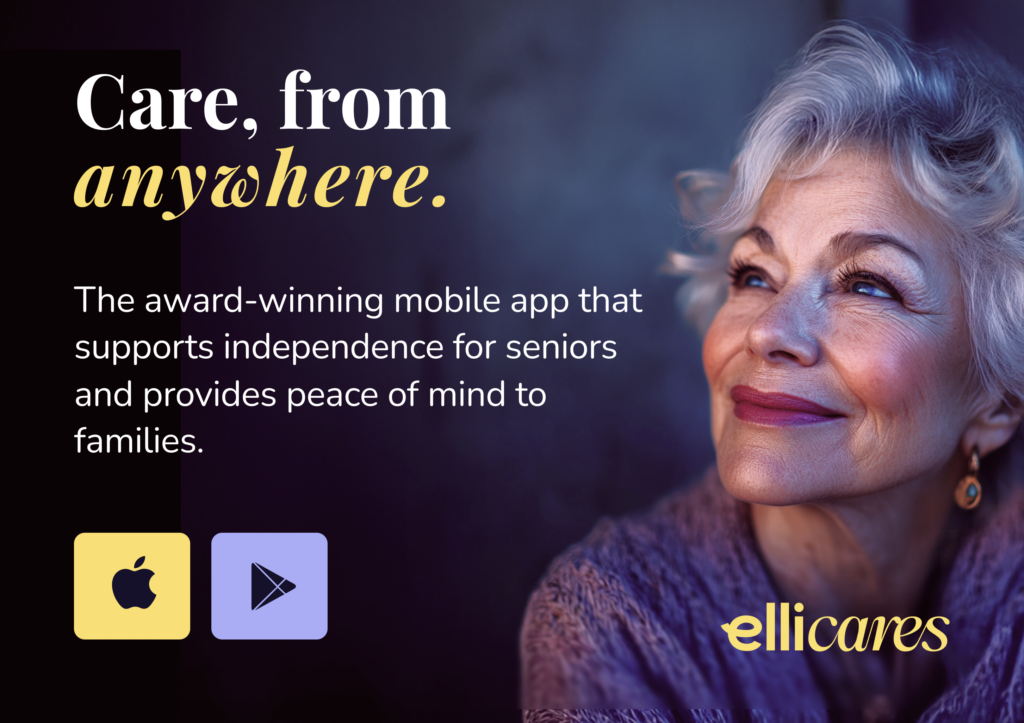
- AI-driven alerts based on behavior changes (like Elli Cares’ Safe Track feature)
- Lifestyle-based interventions like diet, sleep, and mental wellness support
These changes aim to detect problems before they escalate, reducing strain on hospitals and helping people age in place safely.
2. The Rise of Home-Based and Community Care
Healthcare is moving out of hospitals and into homes. According to McKinsey, up to $265 billion worth of care services could shift from traditional facilities to the home by 2025 in the U.S. alone.
This shift benefits aging populations by:
- Offering familiar, comfortable environments
- Reducing hospital readmissions and associated costs
- Allowing technology like remote monitoring, medication reminders, and safe zones to support daily life
3. Technology as a Force Multiplier
With fewer caregivers and health workers available to meet growing demand, technology becomes a force multiplier - augmenting human care rather than replacing it.
Examples include:
- AI-driven chat tools that answer health questions (like Elli’s “Ask Elli Anything”)
- Virtual appointments and telehealth
- Remote medication management systems
- Digital care coordination between family and formal caregivers
But to succeed, this tech must be co-designed with older adults to ensure accessibility and dignity.
👉 Read more about why tech must be co-designed with seniors
4. Workforce Challenges and New Roles
The longevity crisis is also driving the need for new healthcare roles, such as:
- Dementia care consultants
- In-home care tech specialists
- Care coordinators trained in remote monitoring tools
- AI support assistants
Countries like Japan and Germany are already investing in robotic assistance and eldercare training programs to close gaps in workforce availability (BBC).
The Cost of Inaction
If health systems don’t adapt, the cost of aging populations will be steep:
- Overstretched hospitals and care homes
- Burned-out caregivers and medical staff
- Increased mortality from preventable issues
- Economic strain due to rising healthcare costs and reduced workforce participation
The World Economic Forum has flagged the global aging trend as a “megatrend” that threatens to destabilize both economies and public health systems without urgent adaptation.
The Opportunity Within the Crisis
While the longevity crisis presents serious challenges, it also creates an opportunity to rethink how we care for people across the lifespan.
Solutions lie in:
- Empowering older adults with tools that support daily autonomy
- Supporting family caregivers with better resources and shared visibility
- Funding preventative, tech-enabled models of care
- Redesigning infrastructure (homes, communities, policies) to support safe aging
This is not just a health issue - it’s a design, technology, and human issue. One where empathy and innovation must meet.