A dementia diagnosis can feel like a door closing - but it doesn’t have to be. Contrary to widespread belief, people living with dementia can - and often do - live for many years following their diagnosis, especially when supported with the right care, environment, and lifestyle. A recent article from the Times of India challenges the common assumption that dementia inevitably leads to rapid deterioration, instead offering a much-needed perspective rooted in possibility, dignity, and proactive support.
How Long Can Someone with Dementia Live?
There is no single answer. Dementia is not one disease - it’s an umbrella term that includes conditions like Alzheimer’s disease, vascular dementia, Lewy body dementia, and frontotemporal dementia, each with varying rates of progression.
However, experts note that individuals diagnosed in the early stages - especially those with access to consistent care and few other health complications - can live for 10 to 20 years after diagnosis. That means there’s time. Time for joy, routine, connection, and support. Time for families to build new forms of communication and presence.
This insight flips the script from a narrative of loss to one of possibility. But how do we get there?
The Lifestyle Factors That Make a Difference
The article outlines several simple yet powerful lifestyle changes that can improve both quality and length of life for those living with dementia. These include:
1. Nutrition That Nourishes the Brain
Diets rich in antioxidants, healthy fats, and vitamins - such as the Mediterranean diet - are increasingly linked to cognitive resilience. Foods like leafy greens, berries, fatty fish, nuts, and whole grains can support brain and heart health.
2. Staying Physically Active
Movement matters. Daily walking, swimming, or light yoga can improve blood flow to the brain, reduce inflammation, and protect against further decline. Exercise also supports balance, strength, and mood - all critical to maintaining independence.
3. Social and Emotional Connection
Dementia often brings isolation. Yet social engagement is one of the most protective factors for brain health. Whether through family, support groups, religious gatherings, or community activities, regular interaction reduces loneliness, depression, and anxiety.
4. Cognitive Stimulation
Keeping the brain active through puzzles, music, reading, storytelling, or engaging conversation can help maintain neural connections. It’s not about reversing dementia - but slowing progression and supporting retained skills.
5. Managing Other Health Conditions
Controlling blood pressure, cholesterol, diabetes, and depression is key. Many of these chronic illnesses contribute to cognitive decline, especially in vascular forms of dementia. Proper medication adherence and medical oversight are essential.
6. Consistency in Routine
Daily structure helps reduce confusion and anxiety. Predictable routines offer comfort, increase confidence, and allow people to remain engaged in their day-to-day life.
The Caregiver’s Role in Longevity
Perhaps one of the most overlooked factors in dementia longevity is the wellbeing and education of caregivers. The article emphasizes that when caregivers are informed, supported, and not burned out, they are better able to provide compassionate, effective, and safe care.
Caregivers who understand how dementia works - and how it progresses - can adapt communication techniques, build routines that make sense, and anticipate needs in a way that reduces distress for both parties. They can also notice subtle changes earlier, helping to manage symptoms more effectively.
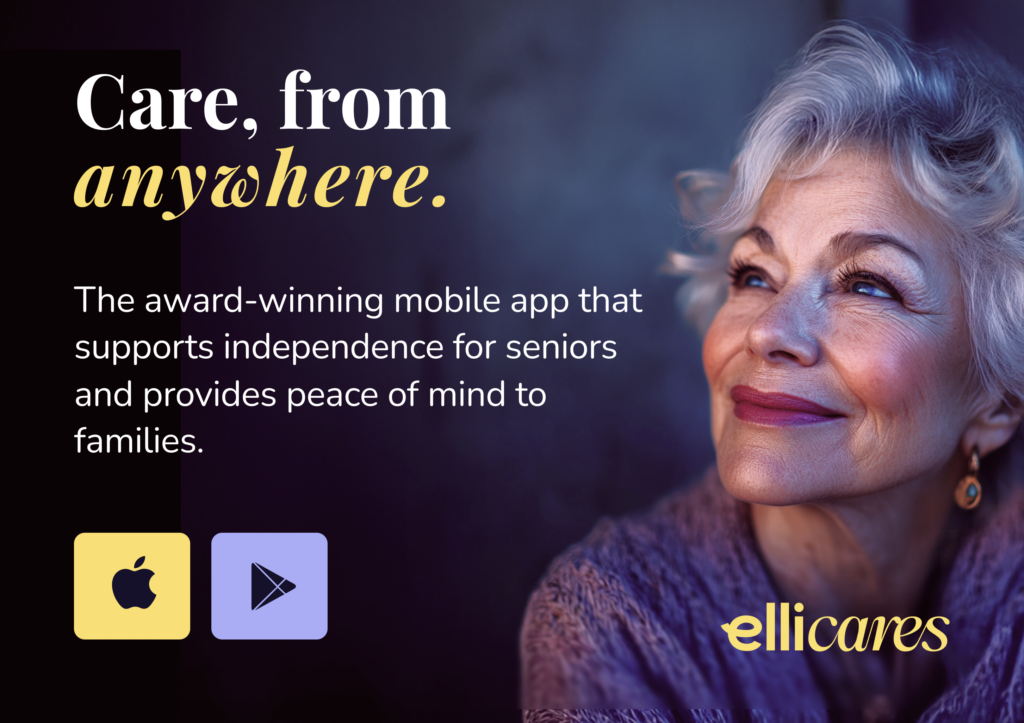
Tools like Elli Cares are designed to ease this burden. With features like reminders, medication prompts, Safe Zones, video check-ins, and care team coordination, the app helps caregivers provide meaningful support - even from a distance. For people living with dementia, these features reduce anxiety, enhance independence, and contribute to overall safety and wellbeing.
A Shift in Thinking: Living With, Not Just Dying From, Dementia
Culturally and medically, we’re slowly shifting from a view of dementia that’s grounded in fear to one that centers on personhood, dignity, and adaptability. That shift is vital, because how we think about dementia affects how we treat people who live with it.
While there’s no cure (yet), there is a great deal we can do to ensure people live longer, better lives - with connection, clarity, and care that evolves with them.
This is the future Elli Cares is building toward: one where technology, empathy, and routine meet in the palm of your hand to provide a lifeline - for both individuals and families. When caregivers feel supported and people with dementia feel understood, we all benefit.
👉 Read the full article on Times of India