Hearing the words Mild Cognitive Impairment (MCI) can bring a mix of emotions: confusion, relief, fear, and hope.
You might wonder:
- Is this the beginning of dementia?
- Can it be reversed?
- What should we do now?
Understanding what MCI means - and taking proactive steps after a diagnosis - can make a significant difference in preserving quality of life and planning for the future.
Here’s what you need to know.
What Is Mild Cognitive Impairment (MCI)?
Mild Cognitive Impairment is a medical condition characterized by noticeable changes in memory, thinking, or judgment that are greater than expected for someone’s age, but not severe enough to interfere significantly with daily activities.
In short:
- There’s clear cognitive change,
- But independence is largely maintained.
Key features:
- Memory lapses (e.g., forgetting recent conversations, appointments)
- Struggling more with planning or problem-solving
- Difficulty finding words
- Feeling mentally "slower" than before
However, people with MCI can still manage their own medications, finances, household tasks, and social life - though they might do so with a bit more effort.
Take a look at the Mayo Clinic's helpful resource on Mild Cognitive Impairment
Does MCI Always Lead to Dementia?
No, not always.
The path after an MCI diagnosis is highly individual:
- About 10-20% of people with MCI progress to dementia each year.
- Some remain stable for years without significant worsening.
- A small percentage even improve - especially if the cause was reversible (e.g., medication side effects, sleep issues, depression).
The biggest risk factor for progression is underlying Alzheimer’s disease or other neurodegenerative conditions.
But even when that’s the case, early action can slow progression and support independence for longer.
What Should You Do After an MCI Diagnosis?
Getting an MCI diagnosis is a powerful early warning system - and an opportunity to take proactive steps.
Here’s what comes next:
1. Follow Up With Medical Care
- Stay in touch with your doctor.
- Regular cognitive assessments can track changes over time.
- Ask about blood tests, brain imaging, or referrals to a memory specialist if not already done.
Sometimes reversible conditions (like vitamin B12 deficiency, thyroid problems, or depression) contribute to cognitive changes - so it's important to rule these out or treat them.
2. Build a Brain-Healthy Lifestyle
Evidence suggests lifestyle changes can support cognitive function and possibly slow further decline.
Focus on:
- Physical exercise: Walking, resistance training, balance work
- Brain engagement: Learning new skills, puzzles, social activities
- Heart health: Managing blood pressure, cholesterol, and blood sugar
- Nutrition: Adopting a Mediterranean-style diet rich in fruits, vegetables, fish, and healthy fats
- Sleep hygiene: Prioritizing 7-9 hours of quality sleep per night
- Stress management: Meditation, yoga, relaxation techniques
👉 Learn more: How to Reduce the Risk of Dementia and Cognitive Impairment
3. Create a Symptom Tracking Routine
Logging small changes can help spot patterns and prepare for conversations with healthcare providers.
Use:
- A simple daily memory and mood journal
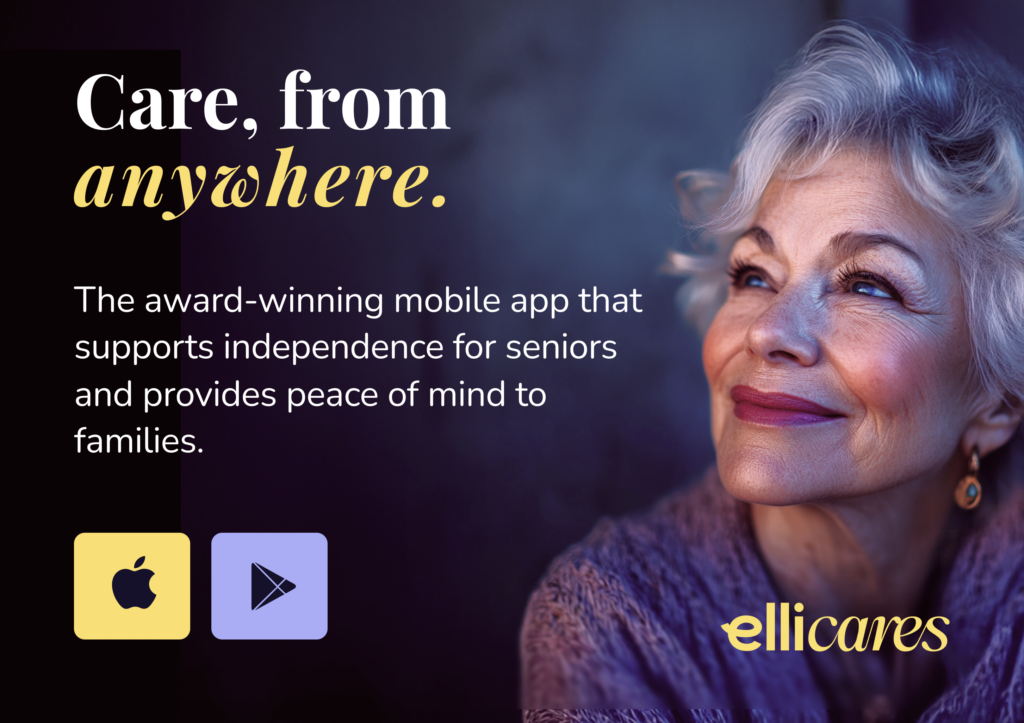
- Mobile apps like Elli Cares to set reminders and track daily health
- Family input for observed changes in behavior or memory
👉 Related reading: Why Seniors Should Track Symptoms - and How to Help
4. Enhance Safety and Daily Organization
Even when symptoms are mild, small adjustments can protect independence:
- Use written calendars and reminder notes.
- Install pill organizers or medication reminder systems.
- Create a safe, clutter-free home environment.
- Set up Safe Zones with Elli Cares if wandering risk is a concern later.
Early support tools build good habits that help if cognitive changes progress.
5. Have Planning Conversations Early
MCI provides an opportunity to make plans while decision-making ability is strong.
Topics to discuss include:
- Advanced care directives
- Financial and legal planning
- Preferences about living arrangements if support becomes needed later
Although these conversations can feel difficult, they reduce future stress and ensure wishes are honored.
Take a look at the Alzheimer's Society's helpful guide on Living With Dementia - Planning Ahead
Emotional Wellbeing After an MCI Diagnosis
An MCI diagnosis can bring anxiety, fear, and sadness. That’s normal.
But it’s important to focus on what remains possible - not just on the uncertainty.
Ways to stay emotionally strong:
- Connect with support groups (online or in person)
- Continue hobbies and social activities
- Celebrate small victories and strengths
- Seek counseling or therapy if needed
Remember: life doesn’t stop with MCI. It simply requires some mindful adjustments.
Final Thoughts
Mild Cognitive Impairment is not the end - it’s a call to action.
A chance to optimize brain health, plan for the future, and embrace support early.
With the right strategies, people living with MCI can continue to lead active, engaged, and meaningful lives for many years to come.
At Elli Cares, we believe early support empowers better living - because brain health is worth fighting for at every stage.